
October 6, 2021 | Volume III, Issue 19

College Celebrates Firestone Building at Ceremonial Groundbreaking
The Larner College of Medicine hosted a ceremonial groundbreaking on September 30, 2021, to celebrate the four-story, 62,500-square-foot Firestone Medical Research Building currently under construction on the southern end of the medical campus. Dozens of people—wearing masks per UVM policy—attended the event in the Hoehl Gallery of the College’s Health Science Research Facility.
“Most of you will have noticed that this is not a traditional groundbreaking,” noted Larner Dean Richard L. Page, M.D., in his introductory remarks. “In fact, construction of the Firestone Medical Research Building began one year ago yesterday, on September 29, 2020. This beautiful building has taken shape, and, thanks to biomedical research leading to vaccines, we are able celebrate this construction, finally, here together.”
In addition to Dean Page, speakers at the ceremony included UVM President Suresh Garimella, Burlington Mayor Miro Weinberger, Marilyn Cipolla, Ph.D., professor of neurological sciences, David Reines, M.D.’72, Firestone Campaign Committee chair and Larner alumnus, and lead donor, alumnus Steve Firestone, M.D.’69.
“In one fell swoop you have helped us satisfy our strategic imperatives,” said President Garimella, addressing Dr. Firestone directly.
Read more about the ceremonial groundbreaking.
Pictured above (left to right): Sarah Lindenfeld, Paquette Building & Construction LLC; Luce Hillman, UVM Facilities Management; Gordon Jensen, M.D., Ph.D., senior associate dean for research; Rick Morin, M.D., former Larner dean; UVM Provost Patty Prelock; Pres. Garimella; Dr. Firestone; Dean Page; Mayor Weinberger; Dr. Reines; Jay Fayette, PC Construction; Keith Robinson, Black River Design. (Photo: Larner Medical Communications).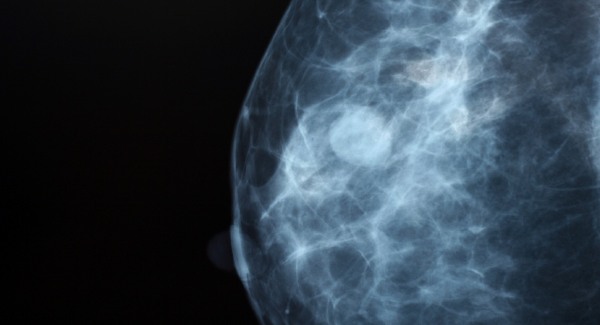
Breast Cancer Care: What We Know Today
Screening
Imaging modalities, like MRI, 3D Imaging, and ultrasound, allow physicians to capture much clearer images of women’s breast tissue, particularly in “dense” breasts, which refers to the amount of fibrous or glandular tissue vs. fatty tissue in a woman’s breast. About half of women over age 40 have dense breasts, which puts them at increased risk for breast cancer. “These types of technologies help us find things earlier and at a more treatable stage,” says Professor of Medicine and Familial Cancer Program Director Marie Wood, M.D.
Medication
Between 2009 and 2018, more than 10 drugs were approved for breast cancer treatment and prevention. “These newer therapies are…specific to the individual’s type of cancer based on the genetic mutations and proteins that are expressed and tend to have less toxicity than traditional chemotherapy,” says UVM Cancer Center Director Randall Holcombe, M.D., M.B.A.
New Treatments
When a patient has cancer, their immune system is suppressed, but by removing blocks in the immune system, patients may be better equipped to fight cancer cells with their own immunity. “We have just scratched the surface on understanding how immunotherapy may be beneficial for patients with triple negative breast cancer,” says Dr. Holcombe.
“For patients with hormone receptor positive breast cancer, we’re also seeing exciting improvements with a number of targeted therapies,” says Peter Kaufman, M.D., professor of medicine and UVM Medical Center oncologist, who adds that the UVM Cancer Center has several clinical trials evaluating both targeted therapies and hormonal medications.
Read more on the UVM Health Network’s “Staying Healthy” blog.
Read a Q&A with Drs. Holcombe and Wood on the UVM Larner College of Medicine blog.
Pictured above: 3-D mammogram image (Courtesy of the UVM Cancer Center.)
Virtual Women's Health and Cancer Conference Draws Nearly 400 Registrants
On Friday, October 1, the UVM Cancer Center hosted its 24th annual Women’s Health and Cancer Conference, which drew a total of 385 registrants, including cancer patients, caregivers, clinicians, researchers, and community members to the free and virtual event sponsored by The Victoria Buffum Fund. Attendees logged into sessions from across the United States, Canada, and as far away as Russia. Nearly a quarter of attendees received continuing medical education credit for their participation.
Conference co-chairs and UVM Cancer Center members Michele Machesky, P.A., a clinician in surgical oncology at UVM Medical Center, and Elizabeth Watson, M.D., M.P.H., assistant professor of radiology, hosted sessions across a broad range of topics. Vermont Commissioner of Health Mark Levine, M.D., provided an intro keynote presentation on the Vermont Cancer Plan and discussed the impact of COVID-19 on cancer care.
Both keynote speaker Rachel Greenup, M.D., M.P.H., of The Breast Center at Smilow Cancer Hospital at Yale, and Electra Paskett, Ph.D., from Ohio State University, spoke about health disparities related to breast cancer care. Dr. Paskett discussed that breast cancer mortality is 41 percent higher in black women than in white women and Dr. Greenup shared research that found 40 percent of white patients compared with 59 percent of black patients have experienced negative financial hardship following their breast cancer diagnosis.
Among the conference sessions was a pre-conference workshop, titled “Having Difficult Conversations,” by Stephen Berns, M.D., associate professor of family medicine, who shared tangible tools for delivering important news to patients and caregivers. Paul Ulager, M.D., assistant professor of family medicine, delivered a widely popular session, titled “Provider Burnout,” which provided research-informed, practical tools for resiliency building. Shahid Ahmed, MBBS, assistant professor of medicine, updated attendees about “Harnessing the Immune System to Fight Cancer,” while Cindy Noyes, M.D., associate professor of medicine, facilitated a panel discussion on “COVID-19 and Cancer” that featured patient and provider perspectives.

– Megan Perkins, Sixth-year Neuroscience Graduate Program student.
Read a recent blog post by Perkins, titled “Graduate School is Tough. But You Can Do It! Here’s How.”
Pictured: Megan Perkins.

Watch the Class of 2025 medical students’ White Coat Ceremony livestream!
Friday, October 8, at 1:00 pm
Watch the live ceremony here.Accolades & Appointments

Polly Parsons, M.D., professor and E. L. Amidon Chair of Medicine, was named a master by the American College of Physicians (ACP). According to the ACP, “Masters shall be Fellows who have been selected because of ‘integrity, positions of honor, impact in practice or in medical research, or other attainments in science or in the art of medicine.’” In addition to being an ACP Fellow, she is also an American Thoracic Society (ATS) Fellow and has served in numerous ATS leadership roles, including as 2018-19 president. Dr. Parsons is the recipient of the ATS Edward Livingston Trudeau Medal, Annual Lifetime Achievement Award, Distinguished Achievement Award, and Elizabeth A. Rich Award. She has long-standing interests in research, education, and patient care and her specific area of research focus is acute lung injury and critical illness.



Professor of Pediatrics Molly Rideout, M.D., recently began a new leadership role as vice chair of medical education in the Department of Pediatrics and the UVM Children’s Hospital. In this newly created position, she is responsible for strategic implementation of the department’s educational mission across the continuum of learning. She is working closely with medical students and graduate medical education leaders in creating, developing and assessing educational programs and courses. A standout teacher and pediatric hospitalist, she most recently served as associate director for pediatric medical student education and director of the fourth-year pediatrics program and the Schweitzer Fellowship Program. She is a Distinguished Educator in the Teaching Academy and this year’s winner of the Outstanding Innovation Award in Curriculum Development for her work creating the Pediatric Concentration for fourth-year medical students. Dr. Rideout serves on the national Executive Committee of the Council of Medical Student Educators in Pediatrics.

CITATION HIGHLIGHTS
Twining PK, Caldwell R, DeSarno M, Blackburn E, Shafritz AB. A 40-year Study of the Factors Associated with Diaphyseal Forearm Fractures in Skiers and Snowboarders. Clin Orthop Relat Res. 2021 Sep 29. doi: 10.1097/CORR.0000000000001982. Epub ahead of print. PMID: 34587121.
Bailey DN, Crawford JM, Jensen PE, Leonard DGB, McCarthy S, Sanfilippo F. Generating Discretionary Income in an Academic Department of Pathology. Acad Pathol. 2021 Sep 23;8:23742895211044811. doi: 10.1177/23742895211044811. PMID: 34595334; PMCID: PMC8477684.
Doyle MF. Central Nervous System Outcomes of COVID-19. Transl Res. 2021 Sep 30:S1931-5244(21)00244-9. doi: 10.1016/j.trsl.2021.09.002. Epub ahead of print. PMID: 34601116.
Uijtdehaage S, Ho MJ, Harvey E, Dorris CS, Huggett KN. Academies in Health Professions Education: A Scoping Review. Acad Med. 2021 Oct 1;96(10):1476-1483. doi: 10.1097/ACM.0000000000004161. PMID: 33983143.
Chen L, Wu N, Kennedy L, Francis H, Ceci L, Zhou T, Samala N, Kyritsi K, Wu C, Sybenga A, Ekser B, Dar W, Atkins C, Meadows V, Glaser S, Alpini G. Inhibition of Secretin/Secretin Receptor Axis Ameliorates NAFLD Phenotypes. Hepatology. 2021 Oct;74(4):1845-1863. doi: 10.1002/hep.31871. Epub 2021 Jul 29. PMID: 33928675.
Schindlbeck KA, Gupta DK, Tang CC, O'Shea SA, Poston KL, Choi YY, Dhawan V, Vonsattel JP, Fahn S, Eidelberg D. Neuropathological correlation supports automated image-based differential diagnosis in parkinsonism. Eur J Nucl Med Mol Imaging. 2021 Oct;48(11):3522-3529. doi: 10.1007/s00259-021-05302-6. Epub 2021 Apr 10. PMID: 33839891; PMCID: PMC8440366.
Sobel HG, Warrington JS, Francis-Fath S, Crocker AM, Berger CA. A Descriptive analysis of urine drug screen results in patients with opioid use disorder managed in a primary care setting. Addict Sci Clin Pract. 2021 Sep 30;16(1):59. doi: 10.1186/s13722-021-00264-4. PMID: 34593036; PMCID: PMC8482571.
Devlin LA, Young LW, Kraft WK, Wachman EM, Czynski A, Merhar SL, Winhusen T, Jones HE, Poindexter BB, Wakschlag LS, Salisbury AL, Matthews AG, Davis JM. Neonatal opioid withdrawal syndrome: a review of the science and a look toward the use of buprenorphine for affected infants. J Perinatol. 2021 Sep 23:1–7. doi: 10.1038/s41372-021-01206-3. Epub ahead of print. PMID: 34556799; PMCID: PMC8459143.
Tsao J, Hook M, Shah P, Bingham PM. Implementation of Pediatric Emergency Care Applied Research Network Guidelines for Traumatic Brain Injury in a Rural Tertiary Care Center. Pediatr Emerg Care. 2021 Oct 1;37(10):513-518. doi: 10.1097/PEC.0000000000002124. PMID: 32541400.
GRANTS REPORT: UVM SPONSORED PROGRAM ADMINISTRATION
Annual/Monthly Reports for Sponsored Projects
WHAT'S HAPPENING
LCOM Events Calendar | UVM Events Calendar | LCOM Student Activities Calendar
Feedback? Contact Us!
View Archive | Subscribe
Published by the Office of Medical Communications
The Larner College of Medicine
at The University of Vermont
Copyright 2021



