Dozens of preceptors, as well as leaders and staff from the Larner College of Medicine and its Longitudinal Integrated Clerkship (LIC) partner Hudson Headwaters Health Network (HHHN), gathered at the historic Queensbury Hotel in Glens Falls, N.Y. for dinner and community project presentations by Class of 2020 medical students Dylon Gookin, Isabella Kratzer, Chad Serels and Collin York on February 20.
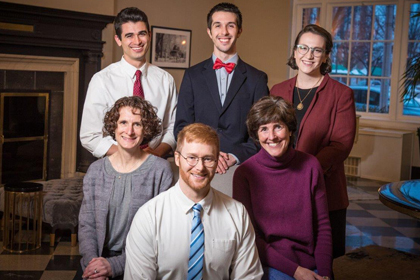
2018-19 Longitudinal Integrated Clerkship students Chad Serels, Dylon Gookin, Isabella Kratzer and Collin York pose with Hudson Headwaters Health Network LIC Site Director Colleen Quinn and Coordinator Jane Morrissey. (Photo: Jim McLaughlin)
Dozens of preceptors, as well as leaders and staff from the Larner College of Medicine and its Longitudinal Integrated Clerkship (LIC) partner
Hudson Headwaters Health Network (HHHN), gathered at the historic Queensbury Hotel in Glens Falls, N.Y. for dinner and community project presentations by Class of 2020 medical students Dylon Gookin, Isabella Kratzer, Chad Serels and Collin York on February 20. The students are finishing up their year-long LIC and will soon transition to their fourth year in a couple of weeks.
For the past nearly 12 months, these students have worked out of a primary care health center “home base” under the supervision of a primary care physician preceptor and have become key members of an interdisciplinary team providing comprehensive care to patients.
Among the attendees at the community projects event were surgeons, pediatricians, family medicine and internal medicine specialists, as well as leaders and staff, including Dean Rick Page, M.D., Interim Senior Associate Dean for Medical Education Christa Zehle, M.D., and Associate Dean for Clinical Education Tania Bertsch, M.D., from Larner, and LIC Site Director Colleen Quinn, M.D., Dominick Bizzarro, president and Chief Operating Officer, and Amy Bloom, executive vice president for network strategy, from HHHN.
First up in the presentation schedule was York, whose community project was titled “How to Improve a Medication-Assisted Treatment (MAT) Program for Opioid Dependence: First, Look at the Evidence.” With guidance from his preceptor, a MAT provider, he examined potential areas for improving access and treatment in a group of 111 patients supported by eight providers. Some of the innovative ideas generated from his project include using telehealth and group treatments to reach more patients, and creating a home induction guide describing how to safely take buprenorphine (Suboxone) at home, with dosing schedules. The parent of a son with opioid use disorder, who is a recovery coach, spoke about the importance of making treatment more accessible in a rural area.
Gookin’s project, titled “Quality Improvement: Cervical Cancer Screening Rates within the HHHN,” was inspired by reports of below-average cervical cancer screening rates among female patients served by HHHN. With an aim to determine and address the cause for these low screening rates, Gookin reviewed a Cochrane meta-analysis of 38 randomized controlled cervical cancer screening trials and found a letter that the UK National Health Services had used for a similar purpose. He then collaborated with HHHN marketing and population health staffers to develop a letter designed to educate women about cervical cancer screening that also invites patients to get screened. It was sent to 1,075 patients. “Patient education is never going to be a bad thing,” said Gookin.
“To JUUL or Not to JUUL: A Crash Course on the Health Effects of Vaping” was the timely topic of Serels’ project. According to his research, 21 percent of the HHHN patient population is dealing with nicotine use disorder and the rate of vaping nationally has risen dramatically over the last few years. Serels then engaged youth from the community in his project, which prompted further research that showed patients relied on their medical providers for information on vaping, yet providers did not feel adequately informed about these products to feel comfortable discussing them with their patients. In response, Serels traveled to health centers across the network giving talks about the health effects of JUUL and other vaping products to providers, nurses, and staff.
The final project presentation, by Kratzer, was titled “Colorectal Cancer Screening Quality Improvement: A FITKit Mailing Initiative.” Kratzer organized mailings of an at-home colorectal cancer screening test and related education that were ultimately sent to hundreds of eligible patients who were not up to date on screenings and hadn’t been to the network’s primary care offices for over a year. While still in the process of collecting data on the returns of the FITKits, Kratzer hopes the mailing program will achieve several important outcomes: eliminate the need for travel to a hospital for screening colonoscopy; access even the network’s most rural populations; and engage a portion of the population that was not receiving regular preventative care. Kratzer and her project were featured in a recent Glens Falls Post-Star article.
Learn more about LIC programs at the Larner College of Medicine at UVM.