Kaminsky and Menson Create COVID-19 Recovery Program
 Members of the Department of Medicine have come together to create a program specifically for patients known as “COVID long haulers,” a group that experiences a constellation of disparate symptoms weeks or even months after initial
infection.
Members of the Department of Medicine have come together to create a program specifically for patients known as “COVID long haulers,” a group that experiences a constellation of disparate symptoms weeks or even months after initial
infection.
Why these patients don’t fully recover from the SARS-CoV-2 virus remains a mystery. According to the National Institutes of Health, symptoms of Long COVID may include fatigue, shortness of breath, “brain fog,” sleep
disorders, fevers, gastrointestinal symptoms, anxiety, and depression. These can “persist for months and can range from mild to incapacitating.” Sometimes, new symptoms emerge late or evolve over time.
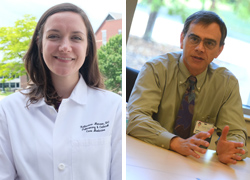
David Kaminsky, M.D.,
(above, at right) professor in the Division of Pulmonary Disease and Critical Care Medicine, says a support group the department created for all UVM Health Network patients diagnosed with COVID-19 helped to identify the need for services
specifically for COVID long haulers. He reached out to colleagues in various divisions, including rheumatology and infectious disease, as well as members of the Department of Family Medicine, to move forward with what is now known as the COVID
Recovery Program.
“None of us felt like we had the critical mass to put together a single clinic that would be staffed solely to see these patients,” he says. “But we realized from the support group that the need
was there nevertheless.”
Katherine Menson, D.O., (above, at left) assistant professor in the Division of Pulmonary Disease and Critical Care Medicine, says COVID long haulers seemed to gravitate to the
support group to lessen their sense of isolation. The recovery program grew from that initial group’s feedback.
“I think one reason that we attract people who've had these symptoms for over a year is because initially they were told that this in their head,” she says. “[They felt] like they weren't heard or listened to. Coming
together with people who have had the same experiences has been helpful for them to feel validated in what they've gone through.”
The group decided to anchor the COVID Recovery Program in the region’s primary care offices.
Specialists worked together to create guidelines for primary care physicians to assess a patient with persistent COVID symptoms and steer them to the appropriate services. Colleagues including Julie Adams, PT, and Suzanne Lawrence, PT, physical
therapists with UVM Medical Center; Jennifer Gilwee, M.D., associate professor and chief of the Division of General Internal Medicine; and Alicia Jacobs, M.D., associate professor in the Department of Family Medicine, collaborated with Kaminsky
and Menson to launch the program.
“If there's severe problems with shortness of breath, they should be referred to pulmonary,” says Kaminsky. “Problems with palpitations or chest pain or dizziness they might go to
cardiology. If the problem is chronic fatigue, muscle weakness, trouble with memory and focus, then they'll go to one of the rehab services, most commonly physical therapy, occupational therapy and speech therapy.”
These long-term therapies seem to pay the most dividends for many COVID long haulers, says Menson.
“We do know that progressive graded physical therapy can help these patients get back toward a functional status that allows them to not be so impacted by shortness of breath, by cough, by brain fog, things like that,” she says.
In addition to getting patients the medical care they need, the program should also help to understand just how many UVM Health Network patients are experiencing Long COVID. It’s a number that has been difficult to pin down here in Vermont and nationally: It is estimated that 10 to 30 percent of patients diagnosed with COVID-19 have some set of symptoms consistent with Long COVID. They are troubling statistics, says Kaminsky.
“Even though Vermont’s overall numbers are low, it still means 30 percent of our patients are potentially going to have persistent symptoms and they're just devastating,” he says. “They're really debilitating, so that's why we need such a program.”
He points to patients who have had to take a leave of absence from work due to the “brain fog” that makes concentration difficult. For some, the symptoms are so severe they have trouble finding the words they need to communicate. Another set of patients can’t maintain the level of physical activity they’re used to thanks to shortness of breath or other respiratory symptoms, which can lead to additional health issues down the road.
A research study from Kaminsky and the Vermont Lung Center, with Menson as a co-principal investigator, seeks to understand more about Long COVID. Funded by the UVM Medical Center Foundation, the study is designed to recruit 50 patients who have been diagnosed with COVID-19, “half of whom have been hospitalized and half of whom do not require hospitalization,” says Kaminsky. The goal is to follow the group for one year, regularly making “detailed measurements of their lung capacity and exercise capacity” to better understand if there are any lingering or subtle changes related to the lungs and COVID.
Although the study is just getting underway, Kaminsky and Menson are excited to uncover more about COVID-19’s disease mechanisms and are grateful to patients volunteering their time.
“Patients have just been so interested in participating as a means to give back and also get answers for themselves,” says Menson.